The knee is one of the most complex and heavily used joints in the body. It relies on multiple ligaments, tendons, and cartilage to provide stability, mobility, and shock absorption. Among these structures, the posterolateral corner (PLC) plays a critical role in stabilizing the knee, especially against rotational forces and varus stress (forces that push the knee inward). A PLC tear is a relatively uncommon but serious injury that can compromise knee stability and function if not properly diagnosed and treated. Understanding the causes, symptoms, and treatment options for a PLC tear is essential for athletes, active individuals, and anyone recovering from knee trauma.
What is a PLC Tear?
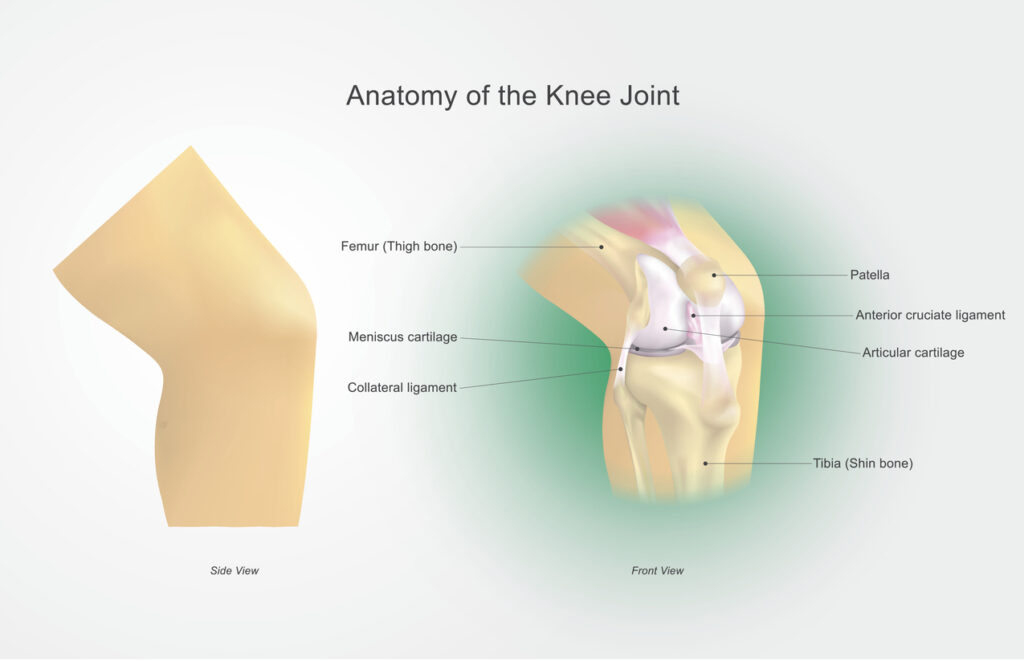
The posterolateral corner of the knee consists of several structures working together to stabilize the joint. Key components include:
- Lateral Collateral Ligament (LCL): Provides side-to-side stability.
- Popliteus Tendon and Muscle: Supports rotational stability and assists in knee flexion.
- Popliteofibular Ligament: Helps prevent excessive external rotation of the tibia.
- Arcuate Ligament Complex and Other Supporting Structures: Contribute to overall posterolateral stability.
A PLC tear occurs when one or more of these structures are damaged, often from high-energy trauma or sports injuries. This type of injury can cause instability, pain, and difficulty performing daily activities or athletic movements.
Causes of PLC Tears
While PLC tears make up only about 2% of all knee ligament injuries, they’re frequently missed or misdiagnosed, especially when they occur alongside ACL or PCL injuries.
The most common causes include:
- Contact Sports Injuries: Football and soccer players who sustain a direct hit to the inside or front of the knee while the foot is planted.
- Skiing Accidents: Falls that force the knee into extreme rotation or outward bending.
- Motor Vehicle Collisions: When the dashboard drives the tibia backward, tearing multiple stabilizers including the PLC.
- Previous Knee Injuries: Patients with untreated ligament tears or chronic instability are more susceptible to secondary PLC damage.
- Repetitive Stress or Chronic Instability: Though less common, repetitive varus stress or previous ligament injuries may weaken the posterolateral corner, making it more susceptible to tearing.
Symptoms of a PLC Tear
Symptoms can vary depending on the extent of the injury and whether other ligaments are involved. Common signs of a PLC tear include:
- Pain on the Outside of the Knee: Pain is often localized to the posterolateral aspect and may worsen with twisting or lateral stress.
- Swelling and Bruising: Mild to moderate swelling may appear after the injury. Bruising is sometimes present along the outer knee.
- Instability or Giving Way: Many patients feel as though the knee “gives out” during walking, running, or changing direction.
- Difficulty Bearing Weight: Severe tears may make it painful or challenging to put weight on the affected leg.
- Reduced Range of Motion: Stiffness or limited ability to fully bend or straighten the knee.
Diagnosing a PLC Tear
Proper diagnosis of a PLC tear requires a combination of a thorough physical examination, imaging studies, and a detailed patient history. During the physical exam, the orthopedic surgeon may perform specific tests such as the dial test, varus stress test, and posterolateral drawer test to assess knee stability and identify which structures are involved. While X-rays cannot directly visualize ligaments, they can reveal associated bone fractures, avulsion injuries, or dislocations. Magnetic resonance imaging (MRI) is considered the standard for evaluating soft tissue injuries, including the LCL, popliteus tendon, and other components of the posterolateral corner. In certain cases, stress radiography may also be used to quantify knee instability under controlled pressure, helping the surgeon determine the severity of the injury and the most appropriate treatment approach.

Treatment Options for PLC Tears
Treatment depends on the severity of the tear, whether other ligaments are involved, and the patient’s activity level. Treatment options fall into non-surgical and surgical categories:
- Rest and Activity Modification: Avoiding high-impact activities and movements that strain the knee allows initial healing.
- Physical Therapy: Focused rehabilitation strengthens surrounding muscles, restores range of motion, and improves overall knee stability.
- Bracing: A hinged knee brace can protect the knee from varus stress while supporting recovery.
- PLC Repair or Reconstruction: Acute injuries may be repaired directly, while more severe or chronic tears often require reconstruction using grafts to restore stability.
- Combined Procedures: If other ligaments, such as the ACL or PCL, are involved, multiple repairs or reconstructions can be performed in a single surgical session.
Risks of Untreated PLC Tears
If a PLC tear is left untreated, it can lead to chronic knee instability, making the knee feel as though it “gives out” during everyday activities or sports. This ongoing instability places additional stress on other ligaments, such as the ACL or PCL, and can accelerate cartilage wear, increasing the risk of early osteoarthritis. Over time, patients may experience difficulty performing routine tasks or engaging in athletic activities safely, and secondary injuries become more likely. Early evaluation and treatment are therefore essential to preserve knee function, prevent long-term damage, and support a safe return to activity.
Preventing PLC Tears
While some knee injuries may be unavoidable due to accidents, sports, or sudden trauma, there are several proactive strategies and lifestyle habits that can help reduce the risk of sustaining a PLC tear. Prevention Strategies Include:
- Strengthen Supporting Muscles: Strong quadriceps, hamstrings, and hip muscles help stabilize the knee during twisting or pivoting movements.
- Practice Proper Techniques: Using correct landing, cutting, and pivoting techniques during sports reduces stress on the knee ligaments.
- Use Appropriate Gear: Supportive footwear and, in some cases, knee braces can protect the knee during high-risk activities.
- Avoid High-Risk Movements: Be cautious when skiing, playing contact sports, or performing activities that place unusual stress on the knee.
- Address Previous Injuries Promptly: Proper rehabilitation of prior knee injuries reduces the risk of recurrent ligament tears, including the PLC.

When to Seek Medical Attention
If you experience knee pain, instability, swelling, or difficulty performing daily activities after trauma or sports injury, it’s important to seek evaluation promptly. Dr. Peter Howard, an orthopedic specialist with expertise in sports medicine and knee injuries, can assess your knee, order appropriate imaging, and develop a personalized treatment plan to restore stability and function. Early evaluation ensures that PLC tears are diagnosed correctly, reducing the risk of long-term complications and helping patients return to their normal activities safely.
Contact Us
The posterolateral corner is essential for maintaining knee stability and function, especially for athletes and active individuals. A PLC tear, though uncommon, can significantly impact mobility and quality of life if left untreated. At Dr. Peter Howard’s practice, patients benefit from advanced diagnostic techniques, surgical expertise, and personalized rehabilitation programs designed to restore knee stability and minimize the risk of future injuries. If you’ve sustained a knee injury or notice persistent instability, schedule a consultation with Peter Howard, M.D., today to take proactive steps toward protecting your knee and maintaining an active, pain-free lifestyle.


